Adult Psychiatry Residency
Saint Elizabeths Hospital/DC DBH places a strong emphasis on training and education at all levels, and the Psychiatry Training Program remains a central component of DBH.
Saint Elizabeths Hospital/DC DBH
Psychiatry Residency Training Program
The Saint Elizabeths Campus is situated in Washington, DC, on heights overlooking the Potomac and Anacostia Rivers. Since it opened its doors in 1855 as the first federal mental hospital, Saint Elizabeths has been a geographical and historical landmark at the center of change in American psychiatry and has been training physicians and psychiatrists throughout its history. It was on this campus the prominent neurologist Dr. Walter Freeman pioneered and hoped to perform on a wide scale his controversial transorbital labotomy, but was stopped by the acting hospital superintendent. It was also here that, half a century later, Dr. Richard J. Wyatt pioneered animal studies in brain transplantation that led to current trials internationally on adrenal transplantation for the treatment of Parkinson’s disease. Working at Saint Elizabeths Hospital, you will be part of a rich legacy involving both historic moments in psychiatry and public controversies. Saint Elizabeths psychiatrists participated in the first battle of forensic experts at the trial of Charles Guiteau, who assassinated President Garfield, and forensic involvement from Saint Elizabeths continued with William Alanson White’s testimony in the Leopold and Loeb trial and Winfred Overholser’s testimony in the case of literary figure Ezra Pound.
The Psychiatric Training Program was formally initiated in 1938. The Department of Behavioral Health places a strong emphasis on training and education at all levels, and the Psychiatry Training Program remains a central component of the DBH. During your training, you will learn the main modalities of psychotherapy (individual, family, and group) and the main psychotherapeutic orientations (psychoanalytic, psychodynamic, cognitive-behavioral, supportive and interpersonal). The campus you walk has been a seedbed for many of these. Staff members of Saint Elizabeths were a major force in introducing psychoanalysis to the public hospital in the last century. The creative arts therapies (art, music, dance, bibliotherapy, and psychodrama) and pastoral counseling have all had pioneering departments on the Saint Elizabeths Campus. These continue to provide invaluable treatment and training services here.
Letter from the Program Director
 Thank you for your interest in Saint Elizabeths Hospital Psychiatry Residency Training Program. Ours is a four-year training program in psychiatry accredited by the Accreditation Council for Graduate Medical Education (ACGME). This program is primarily based at Saint Elizabeths Hospital, which is the public psychiatric hospital for the District of Columbia operated by D.C. Department of Behavioral Health. D.C. Department of Behavioral Health also operates the Mental Health Services Division and the Comprehensive Psychiatric Emergency Program both of which form integral parts of the Residency Program.
Thank you for your interest in Saint Elizabeths Hospital Psychiatry Residency Training Program. Ours is a four-year training program in psychiatry accredited by the Accreditation Council for Graduate Medical Education (ACGME). This program is primarily based at Saint Elizabeths Hospital, which is the public psychiatric hospital for the District of Columbia operated by D.C. Department of Behavioral Health. D.C. Department of Behavioral Health also operates the Mental Health Services Division and the Comprehensive Psychiatric Emergency Program both of which form integral parts of the Residency Program.
Saint Elizabeths Hospital has played a central role in the history and development of forensic psychiatry in the United States and has a Forensic Psychiatry Fellowship program. This hospital also has training programs/internships in psychology, chaplaincy, and dentistry. Five medical schools offer psychiatry clerkships at Saint Elizabeths and we also have an externship program for graduates of medical school looking to gain clinical experience in psychiatry.
Several other institutions including Providence Hospital, Washington DC VA Medical Center, UM Capital Region Medical Center, Whitman-Walker Clinic, George Washington University, Sibley Memorial Hospital, Psychiatric Institute of Washington, University of District of Columbia, and Children’s National Medical Center provide key sites for clinical rotations within this residency training program. Together, these sites offer a wide range of settings where residents work with individuals from a variety of cultural and socioeconomic backgrounds, representing a full gamut of psychiatric disorders.
Our program envisions psychiatry as a field whose origins are firmly rooted in medicine. It is a discipline which integrates neurobiology, psychology, and sociology, each of which deepens our understanding of human behavior and enhances delivery of the best psychiatric care. The rapidly expanding neurochemical and neuropsychological understanding of human behavior is combined with an understanding of human development, psychodynamics and the individual’s social and cultural milieu to cultivate humane care and provide the most effective treatments.
Clinical experience remains the best foundation of psychiatric training. Throughout their training, residents are responsible for the treatment of a wide range of patients. Careful attention is paid to ensure that each resident has extensive longitudinal experience with patients who suffer from chronic, severe mental illnesses as well as patients with significant neurotic and characterological difficulties, which interfere with their personal relationships or occupational functioning. Residents are provided an opportunity to work extensively with adults, children, groups, families, and provide consultation to organizations within the community, all in a supervised setting.
Our training program prepares residents to treat mentally ill population, both as inpatients and outpatients. Many of the most severely mentally ill are involved with the legal system. Circumstances may involve civil commitment, guardianship, and competency to stand trial or legal insanity. The program provides a balanced education with the emphasis on learning psychopharmacology and psychotherapy from accomplished psychopharmacologists and psychoanalysts in the country. Residents are placed in public/private outpatient clinics as well as university student health clinic for outpatient psychiatry experience. The long-standing association between Saint Elizabeths Hospital and the National Institutes of Mental Health (NIMH) provides for elective research opportunities for our residents.
In all, Saint Elizabeths Psychiatric Residency Program provides comprehensive training in all major areas of psychiatric practice with the goal of graduating skilled general psychiatrists. We anticipate that many of our graduates will pursue further training in psychiatric specialties, such as Community Psychiatry, Child and Adolescent Psychiatry, Psychiatric Research, Forensic Psychiatry, Addiction Psychiatry, and Psychoanalysis. All of us at Saint Elizabeths Hospital invite you to explore our training opportunities in psychiatry.
Sincerely,
Farooq Mohyuddin, MD
Director, Psychiatry Residency Training Program
Training & Curriculum
During PGY-1, residents begin to develop skills in assessing and evaluating patients, developing a differential diagnosis, and constructing a treatment plan blending psychopharmacology and other therapeutic modalities. They spend half of the year on various inpatient units at Saint Elizabeths Hospital working as part of a multidisciplinary treatment team. Residents complete their neurology experience, and finally, residents complete their internal medicine experience at one of our affiliated hospitals by working on inpatient teams with internal medicine and family medicine interns.
During PGY-2, residents continue to hone their skills in assessing and evaluating patients, developing a differential diagnosis, and constructing a treatment plan blending psychopharmacology and other therapeutic modalities. With a solid general psychiatry foundation built in PGY-1, the breadth of psychiatry knowledge is expanded as residents rotate through multiple psychiatry subspecialties. Additionally, residents rotate at psychiatry units outside Saint Elizabeths to gain experience of inpatient psychiatry in both the community and government sectors.
During PGY-3, resident are emerged in outpatient psychiatry for the entire year at a variety of clinics throughout the DC community. All PGY-3 residents rotate at the Resident Continuity of Care Clinic, the Children’s National Hospital Outpatient Behavioral Health Clinic, and a third community clinic of their choosing. They build up a case load of patients who they see for pharmacologic management, individual psychotherapy, group psychotherapy, family therapy, couple’s therapy for up to two years.
During PGY-4, residents fine-tune their training skills while taking on stronger roles as leaders and teachers. They are encouraged to develop skills that will help them practice independently after they graduate. Residents’ morning schedules are dedicated to the final required rotations and electives while the afternoons are devoted to continuing outpatient care at the variety of community clinics. This is also the year when usually four residents, chosen by the program, act as Chief Residents and take on additional responsibilities in the areas of program administration, curriculum, wellness, and organization.

PGY-1
Clinical Rotations
Internal Medicine – 4 months
Residents complete this four month long rotation at either University of Maryland Capital Region Medical Center or George Washington University Hospital, both of which have ACGME-accredited Internal Medicine Residency Training Programs. Residents are supervised by internists and medical specialists who spend on average 50% of their time teaching residents. Teaching of interns takes place in seminars, case conferences, floor rounds, and individual or team supervision. Both hospitals are large general hospitals that serve a diverse urban population. Residents have supervised experiences in assessment, treatment, and disposition of a variety of medical illnesses. The goal of this rotation is to improve and advance the level of competency of the residents in the principles of management of the most common medical conditions seen in the general medical wards and outpatient clinics.
Neurology – 2 months
This two month long rotation offers residents an experience in neurology directly relevant to their careers as psychiatrists and, unlike conventional neurology rotations, provides a superb opportunity to evaluate disorders at the interface of neurology and psychiatry. The neurology consultation service on site at Saint Elizabeths Hospital is directed by John Stiller, M.D. and ensures that patients with severe psychiatric disorders are evaluated for comorbid neurologic illness. Residents also rotate at George Washington University Neurology inpatient consultation service. The goal of this rotation is to develop expertise in diagnosis of neurological conditions that might reasonably be expected to be encountered in psychiatric practice and which must be considered in the differential diagnosis of psychiatric disorders.
Inpatient Psychiatry (with ECT/TMS) – 5 months
This rotation comprises of five total months training at Saint Elizabeths Hospital residents spending one or two months on a specific unit under the ongoing supervision of the unit attending psychiatrist. Saint Elizabeths Hospital is a tertiary psychiatric hospital, meaning that patients are only admitted after failing to recover through use of outpatient, emergency, and acute inpatient services. The population of patients residents work with tends to be more severely and chronically mentally ill, often with co-occurring substance use disorders, medical illnesses, and severe psychosocial stressors. On this rotation, emphasis is placed on obtaining a thorough psychiatric and medical history, developing a broad bio-psycho-social differential diagnosis, and developing a comprehensive treatment plan as part of a multi-disciplinary team. This rotation also includes exposure to Electroconvulsive Therapy (ECT) and Transcranial magnetic stimulation (TMS) treatment modalities at Sibley Memorial Hospital.
Inpatient Geriatric Psychiatry – 1 month
This is a one month rotation that takes place on the Inpatient Geriatric Psychiatry Unit at Saint Elizabeths Hospital. On the inpatient geriatric unit, emphasis is placed on evaluating geriatric patients who have often lived with symptomatic mental illness for years or even decades, broadening the differential diagnosis considering conditions of ageing, and adjusting treatment plans to accommodate the biological changes the geriatric population experiences.
Call Shifts
Residents who are completing their six months of inpatient psychiatry experience (including inpatient geriatrics psychiatry) are assigned call shifts to ensure coverage of Saint Elizabeths Hospital outside the hours of 8:00 am to 5:00 pm. Before working call shifts on their own, PGY-1 residents complete training calls with senior residents in order to acclimate them to their responsibilities and the procedures of the hospital. Additionally, a supervising attending psychiatrist is available on-site 24/7 to enrich the learning during a call shift and to address any questions the resident may have.
Short Call (Mon-Fri, 5:00 pm to 8:30 pm)
PGY-1 residents average one short call per week over the 6-month period of inpatient psychiatry. During short call shifts, residents complete admissions, take care of urgent patient care issues on the units, and respond to psychiatric and medical emergency codes.
Long Call (Sat or Sun, 8:00 am to 8:30 pm)
PGY-1 residents average one to two long calls per month over the 6-month period of inpatient psychiatry. During long call shifts, residents round on the hospital units and are once again responsible for urgent patient care issues and psychiatric or medical emergency codes. The hospital does not do admissions on weekends.
Residents who are completing their six months of internal medicine and neurology do not take call shifts at Saint Elizabeths Hospital. During internal medicine, they follow the call schedule set by the internal medicine residency program they are rotating with, which differs based on which hospital they are rotating through for this experience. During the neurology rotation, residents do not have call responsibilities.
The call frequency mentioned above represents an average estimate of monthly calls; however, it may vary for PGY-1 based on the needs of the training and residency program.
Didactics Curriculum
Residents have a full protected day free of clinical duties for didactics based learning as a group. PGY-1 residents on their 6-month inpatient psychiatry experience spend each Wednesday from 8:00 am to 5:00 pm engaging in the courses and seminars listed below.
• Patient interviewing seminar with Dr. S. Kalman Kolansky
• Emergency psychiatric class with Dr. Alican Dalkilic
• Introduction to forensic psychiatry with Dr. Ramia Gupta and Dr. Enrico Suardi
• Prescription Writing and Clozapine REMS with Dr. Hyun Lee
• Child and adolescent development seminar with Dr. S. Kalman Kolansky
• Psychiatric Disorder Seminar with Dr. Lauren Pengrin
• Basic pharmacology with Dr. Volkov
• Group therapy seminar and supervision with Dr. Farooq Mohyuddin
• Communication disorder with Dr. Lauren Pengrin
• Ethics with Dr. Philip Candilis
• ACGME competencies and milestones with Dr. Farooq Mohyuddin
• The effects of sleep loss on performance Dr. Lauren Pengrin
• Psychological testing course with Carla Sterling, Psy. D.
• Introduction to psychotherapy with Dr. Natalia Grekova
• Critical Appraisal of Scientific Literature with Dr. Abhishek Wadhawan
• Introduction to substance use with Dr. Ashwin Mathai
• Biological psychopharmacology with Dr. Muhammad Zaidi
• Neuropsychological testing with Sidney Binks, Ph.D
• Quality Improvement Seminars with Ms. Gillian Laurence
Group Therapy Experience
During the six months of inpatient psychiatry, PGY-1 residents are paired up as co-leaders of a weekly Psychoeducation Group, which takes place at Saint Elizabeths Hospital every Wednesday. The experience of leading a group is complemented with didactics on group therapy dynamics and ongoing supervision by a group psychotherapy trained psychiatrist. The goal is to provide residents with skills in utilizing basic theoretical understanding of the stages of group development, in conducting group therapy, in leading groups and, in applying group methods to a variety of clinical and social situations.

PGY-2
Clinical Rotations
Inpatient Psychiatry – 6 months
For two months at a time, residents rotate on inpatient psychiatry units at Saint Elizabeths Hospital (Community Hospital), Veterans Affairs Medical Center (Federal Government Hospital), and the Psychiatry Institute of Washington (Private Hospital). This allows training experience in a variety of settings that interest residents as they consider their future careers. As a second-year, residents are expected to utilize the foundation they built as an intern to engage in more advanced critical thinking when it comes to patient evaluation and treatment planning. Residents also further their ability to navigate the various systems of mental health care as they continue to function as part of a multidisciplinary system that includes nurses, psychologists, social workers, occupational and recreational therapists, and many others. PGY-2 residents also teach and supervise medical students from various schools who are completing their psychiatry rotations on the inpatient units.
Consultation-Liaison Psychiatry – 2 months
Residents spend two months at either Sibley Memorial Hospital or George Washington University Hospital as members of the psychiatry consultation service. Residents learn the process of psychiatric consultation in a general hospital and the ongoing clinical management of medical and surgical patients who have concomitant psychiatric illness. Under the guidance of psychiatry attendings, residents triage inpatients who are referred to the service and oversee their psychiatric care until they are discharged. Residents are also responsible for coordinating and teaching medical students rotating on the service. During this rotation, residents gain an understanding of the interface between medical and psychiatric disorders, the challenges psychiatric patients can present to their primary care providers, and the effect of medical illnesses on precipitation and augmentation of psychiatric disorders.
Night Float – 5 weeks
During this five week rotation, residents provide on-site overnight coverage (8:30 pm to 8:00 am) at Saint Elizabeths Hospital for six days of the week. Residents are responsible for any evening admissions that are pending when they start their shift, responding to urgent calls from the units, and responding to any psychiatric or medical codes. On weekdays at 8:00 am, the shift ends and they attend the morning report to provide a patient hand-off to the psychiatry residents coming onto the inpatient units for the day. An attending psychiatrist is available on-site 24/7 to take advantage of overnight learning opportunities and support the resident if they need it.
Substance Use Disorders – 5 weeks
This is a five week rotation that gives residents clinical experience with inpatient detox and outpatient recovery. Residents spend part of the time at the Psychiatry Institute of Washington on the detox units performing patient admissions, daily assessments, and discharge planning coordinated with substance abuse counselors. Many patients seen have concomitant mood, anxiety, and trauma-related disorders, giving residents experience with developing comprehensive treatment plans. Residents spend the other part of their time at the Veterans Affairs Medical Center seeing patients in the outpatient Substance Abuse Recovery Program. They perform intakes on patients new to the program, experience recovery support groups, and hold follow-up appointments for established patients in later stages of recovery.
Emergency Psychiatry – 5 weeks
This is a five-week rotation that takes place at the Comprehensive Psychiatric Emergency Program (CPEP), a 24-hour psychiatric emergency room run by the DC Department of Behavioral Health. Patients in acute crisis are brought in either voluntarily or involuntarily, often by the Community Response Team, for emergency mental health evaluation. Residents take part in the triage and psychiatric evaluation of patients and the decision to admit the patient for further observation, refer the patient for medical care or discharge the patient with a plan for outpatient follow-up. Patients who are admitted to CPEP for additional observation and treatment are evaluated daily by residents who also coordinate transfers to acute inpatient psychiatry units if indicated. Skills gained during this rotation include the assessment and management of patients who are a danger to themselves or others, the evaluation and reduction of risk to caregivers, and knowledge of relevant issues in forensic psychiatry.
Call Shifts
PGY-2 residents who are not on their Night Float rotation are assigned call shifts to ensure coverage of Saint Elizabeths Hospital outside the hours of 8:00 a.m. to 5:00 p.m. They also do training calls with our PGY-1 residents in July and January to ensure the new residents are familiar with the responsibilities and the procedures of call coverage. Additionally, a supervising attending psychiatrist is available on site 24/7 to enrich the learning during a call shift and to address any questions the resident may have.
Short Call (Mon-Fri, 5:00 pm to 8:30 pm)
PGY-2 residents average one or two short calls per month over the 10-month period at Saint Elizabeths Hospital. During short call shifts at SEH, residents complete admissions, take care of urgent patient care issues on the units, and respond to psychiatric and medical emergency codes. Second-year Residents are also assigned with short calls at George Washington University Hospital (GWUH) from 6 p.m. to 10 p.m. on Mondays and Thursdays. During the call, residents evaluate patients in the Emergency Department in order to determine admission to the inpatient unit and respond to psychiatric and medical emergencies on the psychiatric unit as well as on the medical floors.
Long Call (Sat or Sun, 8:00 am to 8:30 pm)
Residents PGY-2 average one long call per month over at Saint Elizabeths Hospital. During long call shifts, residents round on the hospital and are once again responsible for urgent patient care issues and psychiatric or medical emergency codes. Second-year Residents are also assigned with one long call every two months at George Washington University Hospital (GWUH) from 7:30 a.m. to 6 p.m. on Saturdays. During the call, residents evaluate patients in the Emergency Department in order to determine admission to the inpatient unit, round on patients admitted to inpatient psychiatric unit, and respond to psychiatric and medical emergencies on the psychiatric unit as well as on the medical floors.
Overnight Call
PGY-2 residents are required to cover the overnight shift on Saturdays on a rotating basis when the night float resident is off duty. Over the course of the year, PGY-2 residents do a Saturday overnight call shift once every two months on average.
The call frequency mentioned above represents an average estimate of monthly calls; however, it may vary for PGY-2 based on the needs of the training and residency program.
Didactics Curriculum
Residents have a full protected day free of clinical duties for didactics based learning as a group. All PGY-2 residents spend each Wednesday from 8:00 am to 5:00 pm engaging in the courses and seminars listed below over the span of the year.
• Addiction Seminar with Dr. Anil Hinnaria
• Neurobiology of Addiction with Dr. Ashwin Mathai
• Ward Management Concepts and Other Topics with Dr. Farooq Mohyuddin
• Consultation – Liaison Seminar with Dr. Robina Niazi
• Biopsychosocial Psychiatry with Dr. John Livingood
• Schools of Psychotherapy with Dr. John Livingood
• Adult Life Cycle with Dr. S. Kalman Kolansky
• ACGME Competencies/Milestones with Dr. Farooq Mohyuddin
• The Effects of Sleep Loss on Performance with Dr. Lauren Pengrin
• Fundamentals of Capacity Assessment: Assessing Medical Decision-Making with Dr. Philip Candilis
• Forensic Psychiatry Lectures with Dr. Ramia Gupta, Dr. Enrico Suardi
• Family Therapy Seminar with Dr. Spencer Ward, Deborah K Ward, LCSW-C
• Couples Therapy and Communication Seminars with Dr. Spencer Ward, Deborah K Ward, LCSW-C
• Resident Process Group with Dr. Spencer Ward, Deborah K Ward, LCSW-C
• Group Therapy and Individual Supervision and Seminar with Dr. Joseph Tarantolo
• Introduction to Psychotherapy with Dr. Natalia Grekova
• Individual Psychotherapy Patients with Dr. Farooq Mohyuddin
• Principles of Psychodynamic Psychotherapy with Dr. Maria Graciela Steiger
• Advanced Psychodynamic Conference with Dr. Steiger
• Ego Psychology and Object Relations with Dr. Bruce Hill
• Quality Improvement Seminars with Ms. Michelle Blake-Smith
Group Therapy Experience
During the year, PGY-2 residents are paired up as co-leaders of a weekly Supportive Psychotherapy Group, which takes place at Saint Elizabeths Hospital every Wednesday. The experience of leading a group is complemented with didactics on group therapy dynamics and ongoing supervision by a group psychotherapy trained psychiatrist. The goal is to provide residents with skills in utilizing basic theoretical understanding of the stages of group development, in conducting group therapy, in leading groups and, in applying group methods to a variety of clinical and social situations.

PGY-3
Clinical Rotations
Adult Outpatient Psychiatry – 12 months (90%)
The goal of this year is to offer an experience for the psychiatry residents in providing continuous care for a variety of adult patients from different age groups, seen regularly and frequently for an extended time in various treatment modalities. Residents spend a total of three days per week in adult outpatient psychiatry clinic, which is split between the Resident Continuity of Care Clinic that is managed by DC Department of Behavioral Health and a second outpatient clinic of their choosing. The faculty is very diverse, representing strengths in psychoanalysis, group therapy, cognitive behavior therapy, family therapy and psychopharmacology.
Resident Continuity of Care Clinic
Residents spend 1.5 days per week at the Resident Continuity of Care Clinic (RCCC). The clinic is one of a few in the community that accepts Medicaid or uninsured patients and includes on-site lab services and pharmacy for those without insurance. The clinic also acts as a psychiatric urgent care where patients can walk-in if they need to establish new care or need urgent care between appointments with their regular psychiatrist. Residents perform full psychiatric evaluations on urgent care patients as openings in their schedule allow. These patients can become part of the resident’s regular case load and be seen for up to two years at the RCCC.
Clinic of Choice
Residents spend 1.5 days per week at a community outpatient clinic of their choice, depending on the type of experience they desire during their outpatient time. Different sites expose residents to varying patient populations, diverse psychotherapy modalities, and supervisors with eclectic professional experience. Currently, there are four clinics for residents to choose from:
Caseload
Resident case load is comprised of patients transferred from recent graduates to provide continuation of care and patients new to the clinic seeking to establish care. Resident caseloads are monitored for diagnostic variety and breadth of treatment experience. The expected breakdown of an average resident caseload includes:
- 8–12 psychotherapy (or combined therapy/medication) patients seen for one hour weekly
- 16-20 pharmacology management patients seen for 30 minutes monthly
- 3-12 patients in a group that meets for one hour weekly
- 1-2 patients seen for full psychiatric evaluation (1.5-2 hours) through the urgent care
Residents are encouraged to see patients who are indicated for a variety of psychiatric treatment modalities. This includes patients indicated for medication management only, psychotherapy only, or combination of medication and therapy. Residents may see patients who are already receiving one type of treatment and are seeking complementary treatment with a psychiatrist. These experiences allow residents to get experience in working with other healthcare professionals to coordinate optimal care for a single patient. Residents interested in specific treatment modalities (e.g. CBT, Family Therapy, Couples Therapy, ECT, TMS, etc.) are encouraged to seek supervision in these areas to better develop these skills.
Supervision
Supervision of pharmacology management appointments generally takes place at the end of each appointment with the on-site attending psychiatrist. Residents are expected to present a summary of the case, including their diagnostic assessment, and explain the reasoning of their medication decisions.
Residents are expected to select supervisors to meet with weekly to process the material from psychotherapy appointments. On average, they should have one hour of supervision for every 2-3 hours of psychotherapy material to be discussed. Supervision can be arranged on an individual basis or in a small group setting. In addition, there is weekly supervision for group psychotherapy built into the didactics curriculum.
Child and Adolescent Outpatient Psychiatry – 12 months (10%)
The goal of this rotation is to provide residents with experience in evaluation and care of the child and adolescent population, exposing them to the broad range of disorders and difficulties seen in these age groups. Residents spend one-half day per week at the Children’s National Medical Center (CNMC) Outpatient Psychiatry Clinic where they see patients for pharmacologic management and psychotherapy. Resident caseloads consist of follow-up patients transferred into their care from recently graduate residents and new patient intakes performed throughout the year. Residents are expected to have one or two long-term psychotherapy patients who they see for up to two years. Supervision for pharmacologic appointments is done at time of appointment by CNMC psychiatry attendings. Supervision of psychotherapy material is done at weekly individual supervision with a psychoanalytic-trained child and adolescent attending psychiatrist.
Call Shifts
PGY-3 residents are assigned call shifts at the Comprehensive Psychiatric Emergency Program (CPEP) in order to gain experience working with patients in acute mental health emergency. Residents take part in the triage and psychiatric evaluation of patients and the decision to admit the patient for further observation and treatment, refer the patient for medical care, or discharge the patient with plan for outpatient follow-up. Call shifts are Monday through Friday from 5:30 pm to 10:30 pm and residents work directly with supervising attending psychiatrists experienced in emergency psychiatry. On average, residents are assigned 2-3 call shifts per month over the course of the year; residents are not on call on DC Government recognized holidays.
Didactics Curriculum
Residents have a full protected day free of clinical duties for didactics based learning as a group. All PGY-3 residents spend each Wednesday from 8:00 am to 5:00 pm engaging in the courses and seminars listed below over the span of the year.
- Outpatient Psychiatry—Introduction, Documentation, Billing, and More with Dr. Monica Acharya and Dr. Lauren Pengrin
- Biopsychosocial Psychiatry Part II with Dr. John Livingood
- Medical Psychiatry and the Neuroscience of Psychiatric Disorders with Dr. Yara Mustafa
- Child and Adolescent Psychiatry and Psychopathology Clinical Cases with Dr. S. Kalman Kolansky
- Child and Adolescent Psychopharmacology with Dr. Enrico Suardi
- Psychiatric Management of Intellectual Disabilities with Dr. Augustus and Dr. Nancy Black
- Advanced Psychodynamic Seminar with Dr. Theodore Fallon
- Principles of Psychodynamic Psychotherapy in Practice with Dr. Maria Graciela Steiger
- Ego Psychology and Object Relations with Dr. Bruce Hill
- Development Focused Brief Psychotherapy with Dr. Sheila Gray
- Cognitive Behavioral Therapy for the Individual and Group with Dr. Philip Scrofani
- Advanced Psychotherapy—Interpersonal Processes and Emotional Regulation with Dr. Philip Scrofani
- Critical Appraisal of Scientific Literature with Dr. Abhishek Wadhawan
- Quality Improvement Seminar with Ms. Michelle Blake-Smith
Group Therapy Experience
During the year, PGY-3 residents are paired up as co-leaders of a weekly psychotherapy group, which takes place at Saint Elizabeths Hospital every Wednesday. Residents have the choice of leading a Cognitive-Behavioral Therapy group or a Psychodynamic-Oriented Therapy group. The experience of leading a group is complemented with didactics on group therapy dynamics and ongoing supervision by a group psychotherapy trained psychiatrist. The goal is to provide residents with skills in utilizing basic theoretical understanding of the stages of group development, in conducting group therapy, in leading groups and, in applying group methods to a variety of clinical and social situations.

PGY-4
Clinical Rotations
Outpatient Psychiatry – 12 months (afternoons)
Residents spend three to four afternoons a week continuing to see their outpatients at the community based clinics they were assigned in the PGY-3 year. This usually averages to one-half day each at the Resident Continuity of Care Clinic, the Children’s National Hospital Outpatient Behavioral Health Clinic, and a third community clinic of their choosing. The fourth afternoon is available for residents to be flexible enough to schedule supervision hours or additional outpatient clinic hours.
Inpatient Junior Attending – 3 months (mornings)
Residents spend three months at Saint Elizabeths Hospital working on an inpatient unit on Monday through Friday mornings. They are assigned to one of three training units where each resident is part of a treatment team, usually comprised of the PGY-4 resident, a medical student, an extern, a social worker, and nursing personnel. The senior resident is the acting attending psychiatrist for a limited number of patients and supervises junior residents, medical students, and externs in developing assessment and treatment skills. The Junior Attending oversees patient evaluations, diagnostic work-ups, and treatment plans that are coordinated with a multi-disciplinary team. Supervision of the Junior Attending is done by the unit attending psychiatrist and the Director of Psychiatric Residency Training, with whom they have one hour of weekly scheduled supervision.
Outpatient Junior Attending (with Homeless Outreach) – 3 months (mornings)
Residents spend three months at the Resident Continuity of Care Clinic working four mornings per week primarily with PGY-3 residents and medical students. At the start of the year, they are responsible for orienting the PGY-3 residents to the outpatient setting. This rotation provides senior residents with experience of the administrative and supervisory roles that attending psychiatrists take on in the outpatient setting. The Junior Attending is responsible for supervising new patient intakes done by the PGY-3 residents by evaluating the case presentation, diagnostic assessment, and proposed treatment plan and providing feedback to the resident. Administrative responsibilities include coordinating the residents’ schedules and urgent care patient appointments, and working with medical students on their psychiatry clerkship.
Residents on this rotation spend their Wednesday morning as part of the Homeless Outreach Program, providing services to homeless adults with psychiatric illness. They are on a team that goes onto the streets, into shelters, and through encampments in order to connect people in need to psychiatric services or multi-service agencies. When indicated, residents help the team perform crisis intervention that may include basic emergency medical care or transporting someone for emergency psychiatric evaluation.
Electives – 6 months (mornings)
Residents are encouraged to develop elective experiences that best meet their developing professional needs and interests. They have two blocks of three month periods that can be used to do two separate electives or one six-month elective.
The following electives are available for residents:
- Inpatient Junior Attending
- Child and Adolescent Psychiatry (many experiences are available for residents through our connection to Children’s National Medical Center)
- Inpatient Child and Adolescent Psychiatry
- Consultation-Liaison Service
- Attention Deficit and Hyperactivity Disorders Clinic
- Gender Development Program (Gender and Autism Program)
- Infant and Toddler Mental Health Program
- Feeding Disorders Program
- Eating Disorders Clinic
- Center for Autism Spectrum Disorders
- Geriatric Psychiatry
- Forensic Psychiatry
- Community Psychiatry
- Administrative Psychiatry
- Emergency Psychiatry
- Addiction Psychiatry
- Electroconvulsive Therapy
- Neurology
- Teaching/Junior Faculty
- Research
Call Shifts
PGY-4 residents are not assigned call shifts during their final year. They do serve as secondary back-up call coverage in the rare case that a resident assigned to call experiences an emergency and the primary resident on back-up is unavailable.
Didactics Curriculum
Residents have a protected half-day free of clinical duties for didactics based learning as a group. All PGY-4 residents spend each Wednesday from 1:00 pm to 5:30 pm engaging in the courses and seminars listed below over the span of the year.
- Psychiatric Topics Roundtable with Dr. John Livingood
- Case Conference Seminar with Dr. Sheila Gray
- Psychiatric Administration and Financing with Mr. Mark Chastang
- Integrated Care Curriculum with Dr. Natalia Grekova
- Child and Adolescent Case Conference and Literature Review with Dr. S. Kalman Kolansky
- Spirituality/Religion and Psychiatry with Dr. S. Kalman Kolansky
- Homelessness Seminar with Jordan Gulley, LICSW
Residency Academic Activities
Journal Club
Each resident hosts a lunchtime journal club meeting once during their time in the program which is attended by peers and faculty. The resident is paired with a supervising faculty member who oversees the selection and preparation of a peer-reviewed journal article to be presented and critiqued. This experience is aimed to teach residents how to critically review publications in order to determine how new scientific information may influence their clinical practice.
Resident Case Conference
During the four year program, each resident is scheduled for a case conference during which they present an interesting patient to peers and faculty. The resident selects a faculty member to work with on developing the case presentation and to facilitate discussion during the conference. Topics in the past have included neurologic causes of psychiatric symptoms, patients with complex differential diagnoses, and psychotherapy case formulations.
Multidisciplinary Case Conference
As a teaching hospital, Saint Elizabeths Hospital is home to multiple training programs including psychiatry, psychology, dentistry, art and music therapy, chaplaincy, and nursing. This unique setting allows residents to take part in multidisciplinary case conferences, during which a patient case is presented by trainees from all available training programs. Psychiatry residents present the case history and treatment from a medical-psychiatric perspective while learning how other evaluation and treatment modalities complement the patient’s healing process.
Scholarly Project
Completing a scholarly project is a graduation requirement for all psychiatry residents in the program. This is ideally, a publication in a scientific journal or a poster/oral presentation at a national or regional professional meeting. At the yearly Overholser Research Day at Saint Elizabeths Hospital, residents are expected to summarize their scholarly project in a presentation and display their poster, if applicable.
Salary
Effective October 6, 2024
- PGY-1 – $66,976.00 + $2500 New Resident Differential (one-time PGY-1 allowance)
- PGY-2 – $72,565.00
- PGY-3 – $75,663.00
- PGY-4 – $80,480.00
- Chief – $86,947.00
Resident salary increases are determined every three years through collective bargaining between the residents and the District of Columbia.
The residency program also provides:
- $1250 yearly stipend for books and educational materials for all residents
- $1000 on-call allowance for PGY-1/PGY-2 and $500 for PGY-3/PGY-4
- $500 reimbursement eligibility for conference/training attendance (presentation not required)
- $1850 reimbursement eligibility for conference/training presentation (pursuant to DBH referral and funding)
- One physician’s white lab coat and one set of scrubs
- PC laptop and Android phone for use during residency training.
Benefits & Discounts
Our residents are employed by the District of Columbia, which means they have access to numerous employee benefits and discounts.
Benefits
- Health insurance: DC pays 75% of premium
- Dental insurance: DC pays 100% of premium
- Vision insurance: DC pays 100% of premium
- Paid Family and Medical Leave (up to 8 weeks)
- Inova Employee Assistance Program
- Residents can use this program to get direct assistance or referrals for a variety of services including confidential counseling, legal services, financial services, child care, elder care, and work-life services.
- Deferred Compensation Plan
- Reimbursement of parking at clinical sites and mileage between sites
Optional benefit programs available for residents to enroll in include:
- Healthcare Flexible Spending Account
- Dependent Flexible Spending Account
- Short-Term and Long-Term Disability Insurance
- Term Life Insurance (DC pays 1/3 of premium)
- Employer-Assisted Housing Program
- DC College Savings Plan
- Savings Bond Program
Discounts
Health & Wellness | Technology | Travel | |
|
|
| |
Entertainment | Work-Life | ||
|
| ||
Leave
Residents have a variety of leave options to use in order to maintain a healthy work-life balance while in residency training:
- 13 days of annual leave per year for personal time off
- 13 days of sick leave per year for health appointments and emergencies
- 10 days of exam leave per year for licensing exam preparation and completion
- 7 days of education leave per year for attending conferences and training
- 5 Wellness days for residents to focus on their overall well-being, including their physical, mental, and emotional health.
- 11 paid DC Government recognized holidays off per year
Resident Life
Residents in our program frequently find time to pursue personal interests like volunteer work, special interest groups, or travel. The Social Committee, composed of residents from each year, plans monthly social events for residents, and seasonal gatherings are put on by the program leadership. Our residents also enjoy spending time together attending conferences around the country.
Fall Welcome
Residents and faculty gather every fall to welcome the new intern class and celebrate with continuing residents. This is generally a pot luck style dinner event that has generally been hosted at one of the faculty homes. Last year, the fall welcome occurred in November and was a thanksgiving gathering with two turkeys and side dishes made by residents and faculty.


Mardis Gras Party
Residents and faculty enjoyed a pot luck style Mardis Gras celebration with king cake, beads, and masks.
Residents’ Day
Every spring, a day is dedicated to the residents to spend free of clinical duties so they can relax and bond. Residents contribute ideas of activities for the day and the Chief Residents work with the program leadership to plan a day of fun. Past activities have included morning yoga, duckpin bowling, a trip to the DC Museum of Modern Art, an afternoon of outdoor activities at a park, and a bubble ball competition.





Social Gatherings
Residents meet throughout the year for holidays and special events to celebrate together. In the past few years, they have celebrated the 4th of July with fireworks, the winter holidays with an ugly sweater party, and the end of the academic year with a pool party.


DC MindGames
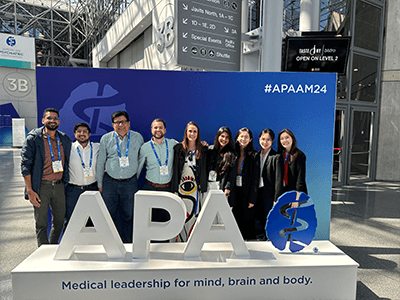
MindGamesis APA’s national residency team competition for residents to test their knowledge on patient care, medical knowledge, and psychiatric history. Each year, the psychiatry residencies in DC send a team to compete on behalf of their program. The residents from Saint Elizabeths Hospital have brought home the trophy for the past four years.
Attending Conferences





Hanging Out Around DC






Clinical Training Sites
Residents complete a large amount of their clinical training at Saint Elizabeths Hospital, which provides a strong inpatient psychiatry experience. Different clinical sites within the DC Department of Behavioral Health offer training experience at various levels of care from acute emergency intervention to long-term outpatient care. Additionally, residents rotate through other hospitals and clinics in DC to build upon their already comprehensive training experience.
Saint Elizabeths Hospital
Inpatient Psychiatry, Geriatric Psychiatry, Neurology, Night Float, Inpatient Junior Attending
35 K Mental Health Clinic
Adult Outpatient Psychiatry (includes Urgent Care), Outpatient Junior Attending
Comprehensive Psychiatry Emergency Program
Emergency Psychiatry
The George Washington University Hospital
Internal Medicine, Neurology, Consultation-Liaison Psychiatry
University of Maryland Capital Region Medical Center
Internal Medicine
Sibley Memorial Hospital
Geriatric Psychiatry (ECT/TMS), Consultation-Liaison Psychiatry
The Psychiatric Institute of Washington
Inpatient Psychiatry, Addiction Psychiatry
DC Veterans Affairs Medical Center
Inpatient Psychiatry, Addiction Psychiatry, Adult Outpatient Psychiatry
University of the District of Columbia
Adult Outpatient Psychiatry
Whitman – Walker Clinic
Adult Outpatient Psychiatry
Providence Health Services
Adult Outpatient Psychiatry
Children’s National Medical Center
Child and Adolescent Outpatient Psychiatry
Prospective Applicants
Our psychiatry residency program is looking to accept MD or DO candidates to start on July 1, 2025 through the Main Match of the National Resident Matching Program (NRMP). All applications must be submitted through the Electronic Residency Application Service (ERAS). All candidate interviews will be held virtually for the 2024 – 2025 ERAS season.
Important Dates
June 5, 2024 | ERAS 2024 season begins at 9 a.m. ET. |
Sept. 4, 2024 | Residency applicants may begin submitting MyERAS |
Sept. 25, 2024 | Residency programs may begin reviewing MyERAS |
October 2024 through January 2025 | Applicant interviews will be held virtually. |
Jan 31, 2025 | The latest date for applications for 2025 residency match cycle. |
Feb 3, 2025 | Ranking opens for applicants and programs |
March 05, 2025 | Rank Order List Certification Deadline for applicants and |
March 17, 2025 | Beginning of Match Week and Supplemental Offer and Acceptance Program® (SOAP®) . |
March 21, 2025 | Matchday! |
Selection Criteria
In order for a candidate to be accepted to the program, they must meet the required criteria below:
- Candidate must have at least one of the following credentials:
- Graduate of a medical school in the United States or Canada accredited by the Liaison Committee on Medical Education (LCME),
- Graduate of a college of osteopathic medicine in the United States accredited by the American Osteopathic Association (AOA),
- Graduate of medical schools outside the United States and Canada who have passed USMLE Step 2 CK and are expected to obtain an ECFMG certificate before their appointment.
- Graduate of a medical school outside the United States who have completed Fifth Pathway program provided by an LCME-accredited medical school
- Candidate must have excellent communication skills in written and spoken English.
- Candidate must have a broad interest in the human condition and be sensitive to cultural issues, psychologically minded, and curious about psychological functioning.
- Candidate must present at least 3 letters of recommendation from physicians or supervisors familiar with their work.
- If more than 5 years have elapsed since graduation from medical school, USMLE Step 3 must be successfully passed.
The following criteria are highly desirable but not required for acceptance:
- Graduated from medical school in the past 5 years
- No failures in USMLE/COMLEX combined history (one failed grade is acceptable if the Step 2 CK score is above 210)
- If graduated from medical school more than 5 years ago, have been involved in continuous clinical or research experience since graduation, preferably some in the US and/or postgraduate training in psychiatry
- Passed USMLE Step 3
- USMLE Step 2 CK score above 220 or COMLEX Level 2 CE score above 500
- Research or clinical experience/publications
- Clinical experience in the field of psychiatry with one letter of recommendation from a psychiatrist who has been a clinical supervisor
- Creative interest in psychiatry, psychological mindedness, and integration of personal experience with the desire to become a psychiatrist
- Language skills in addition to English
Applications
Applications are accepted starting in September and are preferred by November 1. Interviews are by invitation only and are a required component of the application process. Interviews are scheduled at the mutual convenience of the applicant and the program between November 1st and January 31st. The interview day is designed to provide applicants with exposure to different aspects of our program and to meet some of our residents and faculty.
Interested applicants who meet the required criteria should send the following documents to the program via ERAS:
- Dean’s letter/Medical School Performance Evaluation (MSPE)
- Transcript
- Personal Statement
- USMLE or COMLEX examination scores
- Three (3) Letters of Recommendation
- Curriculum Vitae
- ECFMG Certification, if applicable
International Applicants
Our residency program accepts qualified applicants with the following visa statuses:
- J-1 visa sponsorship through ECFMG
- H-1B visa
Contact Us
Further inquiries regarding the application process should be directed to:
Reetika Morgan
Psychiatry Residency Program Coordinator
Saint Elizabeths Hospital/DC Department of Behavioral Health
1100 Alabama Ave SE, Ste 238
Washington, DC 20032
Tel: (202) 299-5334
Fax: (202) 561-6953
E-mail: seh.psychres@dc.gov
Psychiatry Residency Program Directors & Staff
Farooq Mohyuddin, MD, CGP, FAPA
Chair of Psychiatry Training, Psychiatry Residency Program Director
Farooq Mohyuddin, MD, CGP, FAPA, is the Chair of Psychiatry Training and Director of Psychiatry Residency Training Program at Saint Elizabeths Hospital. Dr. Mohyuddin is a medical graduate of Sindh Medical College, Karachi, Pakistan, Class of 1989, and completed his training in Psychiatry at Saint Elizabeths Hospital, Washington, D.C. in 2003. He has served as the Director of Medical Student Education at Saint Elizabeths Hospital, President of the Mid Atlantic Group Psychotherapy Society, Chair of Group Psychotherapy Training Program, and the President of Washington Psychiatric Society. He is an active Member of Administration and Leadership Committee, Group for the Advancement of Psychiatry. His interests include teaching, group psychotherapy, and psychopharmacology.
![]()
Janna Volkov, MD
Psychiatry Residency Associate Program Director
Janna Volkov, MD, is Associate Program Director at Saint Elizabeths Psychiatry Residency Training Program. She is the Director of Medical Student Education and Psychiatry Externship Program. Dr. Volkov is a medical graduate from Novosibirsk State Medical Academy, Russia. She completed her training in psychiatry at Saint Elizabeths Hospital, Washington, DC. Dr. Volkov is a Clinical Assistant Professor of Psychiatry and Behavioral Sciences at George Washington University School of Medicine and Health Sciences, as well as an adjunct professor of clinical psychiatry in the Department of Psychiatry and Behavioral Sciences at Howard University. Her clinical experience includes working as an ACT team psychiatrist and an outpatient psychiatrist at the Department of Behavioral Health. As the director of the outpatient resident’s clinic, she supervised PGY-3 and PGY-4 residents for medication management and psychotherapy. Dr. Volkov is a PGY-1 year supervisor who teaches psychopharmacology, psychiatric interviews, and case conference seminars. She is also a psychotherapy supervisor. Her interests include teaching, individual psychotherapy, psychopharmacology, and community psychiatry. Her research interests include seasonal affective disorders, sleep medicine, and the correlations between suicidal behavior, depression, and seasonal allergen exposure.
![]()
S. Kalman Kolansky, MD, DLFAPA
Psychiatry Residency Associate Program Director
S. Kalman Kolansky, MD, DLFAPA is a graduate of Georgetown University School of Medicine, 1965. He provides education and supervision in child and adolescent psychiatry and development throughout the four years of residency. Dr. Kolansky completed his psychiatry residency at Kings County Hospital, Downstate Medical Center, Brooklyn, NY, and Child Psychiatry Fellowship Training at Hahnemann Medical School and Hospital Philadelphia, PA. He is a Teaching Psychoanalyst at the Washington Baltimore Psychoanalytic Institute and Assistant Clinical Professor of Psychiatry at George Washington University School of Medicine. He is the recipient of the Irma Bland Teaching Award from the American Psychiatric Association, and the Edith Sabshin Teaching Award from the American Psychoanalytic Association. He is also a Distinguished Life Fellow of the American Psychiatric Association. His interests include child development pre-school consultation, individual psychotherapy and psychoanalysis of children, adolescents, and adults, psychological effects of adoption and foster care on the adoption triad, psychoanalysis and cinema, and psychological trauma through the life cycle. Dr. Kolansky is also in part-time child, adolescent, and adult psychiatry and psychoanalytic practice in Alexandria Va.
![]()
Reetika Morgan
Psychiatry Residency Program Coordinator
![]()
Michelle Singletary
Psychiatry Residency Program Specialist
![]()








